Breast Augmentation
Mammary hypoplasia is defined as a breast volume which is insufficiently developed in proportion to the patient’s morphology. It can be a pre-existing condition (small breasts from puberty) or appear later, after substantial weight-loss, a pregnancy followed by breast-feeding, or hormonal problems.
It can occur alone or be associated with ptosis, which is sagging of the breasts and skin stretching and a lowered areola.
This insufficient breast volume is often a source of physical and psychological distress for the patient who feels she lacks femininity, with also a lack of self confidence and poor self-image which can lead to an inferiority complex. Breast augmentation with implants is the solution to these problems.
The procedure can be carried out at any age above 18, below this age the procedure is not advisable.
The implants used at present are composed of a shell and filler. The shell is always made of silicone rubber, but the filler can vary. The implant is termed ‘pre-filled’ when the filler was inserted during the manufacturing process (gel and/or saline solution). The different volumes are therefore fixed by the manufacturer. Implants filled with saline solution are filled by the surgeon who can adapt them to the patient to a certain extent during procedure.
New Generation Pre-Filled Silicone Gel Implants
The great majority of implants used in the world are pre-filled silicone gel implants.
These implants, which have now been used for over 40 years have been proved to be safe and to be the best product for this procedure since they are very close to the consistency of a normal breast. There has been great progress in this domain since the late 1990’s; any weak points have been eliminated.
They are made of soft silicone gel inside a strong impermeable envelope of silicone rubber which can be rough or smooth.
The most important points concerning the new generation of implants, which ensure their safety, are the new improved envelopes and the gel itself.
The shells, which are now stronger, prevent any leakage of gel (which was a cause of capsule formation) and have much greater resistance over time.
Cohesive silicone gel which has a thicker consistency will not spread in case of rupture of the envelope.
Added to this increased reliability is the fact that this new generation of silicone implants exists in different shapes, making it possible to adapt them to individual needs. Thus we find, in addition to the classic round implants, anatomic ‘teardrop’ shapes which can be higher, wider or more pointed.
This diversity of shape, associated with a range of volumes means that the choice of implant can be tailored to the figure and the expectations of the patient.
Other Types of Implants
The envelope is always silicone rubber; it is the filler which can be different:
Physiologic saline: This is in fact salt water (which makes up 70% of the human body). These implants can be ‘pre-filled’ by the manufacturer or ‘inflatable’ that is, filled by the surgeon during the procedure. Since the filler is a liquid rather than a gel the breasts do not feel natural, the implants can wrinkle, which can be palpable or even visible; they can also deflate suddenly even after a short time.
Before The Procedure
After discussion between the patient and the physician who will have clearly explained the different options the best choice for each case is agreed on during the preoperative consultation taking into account all the relevant parameters ( height, weight, pregnancies, breast feeding, body shape, body fat, size of the existing breasts, muscle tone...).
After studying these parameters and anatomic features of the patient, the surgeon will determine the plan for the operation. This will also take into account his preferred technique and the expectations of the patient and the positioning of the scars, the type and size of implants, and the position of the implants above or below the muscle.
A thorough preoperative examination with blood tests will be carried out as prescribed.
An anesthesiologist will see you in consultation at the latest 48 hours before the operation. In addition to the usual preoperative tests it can be helpful to use medical imagery, (mammography, and echography).
No aspirin-based medication should be taken during the 10 days preceding the operation & 3 days after surgery.
Stop smoking is recommended at least one month before and 6 weeks after the intervention (smoking can cause a delay or bad healing & others).
Hospital Stay and Type of Anesthesia
Type of anesthesia: This is usually classic general anesthesia; you will sleep throughout the operation.
Hospital stay: One day in hospital is usually sufficient. The patient arrives in the morning and leaves the next day. However the procedure can be carried out in an ambulatory setting, the patient leaves after some hours of medical supervision.
The Procedure
Each surgeon has adopted his or her own specific technique, which he or she adapts in order to obtain the best results in each case.
We can however give some basic points:
The Incisions
There are several possible approaches:
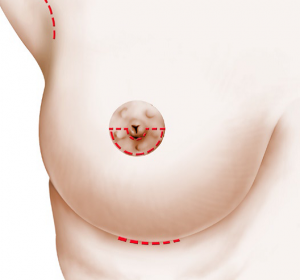
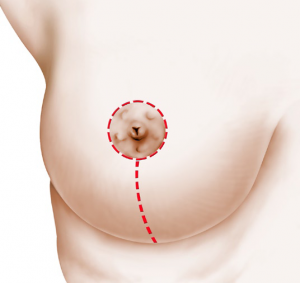
Peri-areolar and intra-areolar approach (around the areola) the incision is either below the circumference of the nipple or horizontal to the nipple.
- Axillary approach
The implant is inserted through a small incision situated in the armpit, or in - The inframammary approach
The incision is in the inframammary fold.
These incisions correspond of course to the position of future scars which will thus be hidden in natural folds or lines.
The position of the implant
This can be in a pocket made in the breast tissue behind the mammary gland and in front of the pectoral muscle, or behind both the mammary gland and the pectoral muscle.
The choice of position will have been predetermined with your surgeon.
• Implant in front of the muscle,
• Implant behind the muscle; gland
The choice of position will have been determined in consultation with the surgeon.
Additional surgery
In case of ptosis (sagging breasts, a lowered areola), it is appropriate to associate a breast lift (mastopexy); this implies.
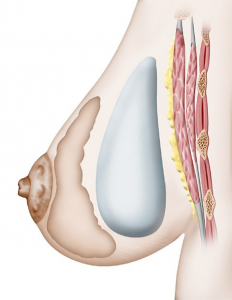 Pre-muscular implant |
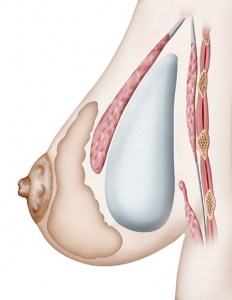 Retro-muscular implant |
Drains:
A drain may be left in place for a few days after the procedure in order to evacuate any blood or liquid which may form around the implant.
At the end of the procedure a special surgical”bra” is put in place.
The length of the procedure varies with each surgeon and of course lasts longer with additional surgery but in general the operation lasts one to two and a half hours.
After The Operation
There can be pain for the first few days after the procedure, particularly when the implant is large and/or placed behind the muscle. In this case pain medication is necessary to dull the pain and prescribed for several days.
Even if there is no pain there will be a strong sensation of tightness.
Swelling and bruising of the breasts and difficulty in rising the arms are frequent immediately after surgery.
The surgical bra can be recommended to be worn night and day for 4 weeks.
If the stitches are non-absorbable they will be removed several days after surgery.
Five to 10 days convalescence is necessary before returning to work.
Patients are advised to wait for one to two months before practicing any sports.
The Result
This can be truly seen from two to three months after surgery, the time necessary for the breasts to become softer and for the implants to settle. The procedure will have improved not only the volume but the shape of the breasts. The scars are usually hardly visible. The added breast volume affects the figure in general; this means that more elegant clothes can be worn.
Added to this aesthetic improvement there is usually a positive psychological effect due to enhanced femininity.
Duration of results
The implants have their own life-span, (see below) but without taking this into account the result of this procedure concerning volume, is long-lasting. The exception can be when a patient puts on a lot of weight. It is true however the shape and firmness of the ‘enlarged’ breasts will suffer, like ordinary breasts, from the effects of aging and gravity which cause drooping, more or less rapidly according to age and support quality of the skin, and also the volume of the implants.
Disappointment Results
The following problems can occur occasionally:
• Asymmetry of the final volume in spite of the use of different sized implants to correct the problem.
• Stiffness with insufficient softness and mobility (especially with larger implants).
• An artificial appearance especially for very slim patients, the upper limit of the implant is visible.
• The implant can be detected when touched especially when the thickness above the implant is reduced (skin + fat + gland) and when the implant is large.
In cases where the patient is not satisfied with the result certain problems can be corrected by revision surgery after a few months.
Frequently Asked Questions
Pregnancy/breastfeeding
After having this procedure there is no problem regarding pregnancy either for the mother or the child, but it is advisable to wait for six month after surgery. Breastfeeding is still possible in most cases.
Auto-immune disease
Many international research papers published on the subject have shown that there is not a higher risk of contracting this type of rare disease with implants compared to the general female population.
Implants and breast cancer
To our knowledge at present we can affirm that breast implants, including those filled with silicone, do not increase the risk of breast cancer. However, during screening techniques clinical examination and palpation can be affected, especially in case of siliconoma or capsular contraction. The presence of the implants can also make it difficult to carry out and read routine mammography. It is necessary to explain beforehand that you have implants. Other radiological techniques can be used; echography, MRI etc. Furthermore, if there is doubt as to a diagnosis of breast cancer you must be aware that more invasive exploratory techniques may be used in order to be sure of the result.
How long will the implants last?
Although it is true that some patients can keep their implants for decades without major changes, an implant, whether filled with silicone gel or saline, cannot be said to last for a specific time, this is not a permanent life-long prosthesis. A patient with implants must expect them to be replaced at some point in time, if the initial effect is to be maintained. It is impossible to predict the life-span of an implant, of whatever type, as this depends on wear which is variable.
This means that no guarantee can be given regarding their life-span.
It should be noted however that the new generation implants are far more hardwearing and reliable. The notion of replacement after ten years is no longer justified, they only need to be replaced if a problem is detected, or the patient wishes to change their size or shape or to correct ptosis
Follow up It is important to keep the appointments with your surgeon during the weeks and months following the operation. After this stage regular medical visits with, for example your gynecologist, or for routine mammography will continue this follow up. You must tell each physician that you have breast implants.
A specific visit concerning the implants is advisable every two to three years, but in case of a change observed in a breast, or an accident affecting the breasts, an appointment must be scheduled.
Possible Complications
Breast augmentation with implants, although essentially an aesthetic procedure is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
A distinction should be made between risks related to the anesthesia and those related to the surgery.
For the anesthesia, the anesthesiologist will explain the risks during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control: the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible.
In fact, techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the surgery is elective and the patient is in good general heath.
Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks to a large extent, without however eliminating them completely.
In general after augmentation mammoplasty the recovery period is straightforward. There can however be complications some of which are inherent to all breast surgery, some linked to the placing of a foreign body in the breast: that is to say risks linked to implants.
1/ Possible complications inherent to all breast surgery:
• A hematoma: blood can surround the implant shortly after surgery. In case of heavy bleeding it is necessary to return to the operating room to drain the blood and put a stop to the bleeding.
• Seroma: this means an accumulation of lymphatic liquid around the implant. It is a frequent complication often associated with considerable swelling. It gives rise to a temporary increase in the volume of the breast or breasts. It decreases gradually and disappears.
• Infection: rare after this procedure. It can require more than one course of antibiotics and the removal of the implant for several months following drainage. After this time interval another implant can be put in place.
Three types of infection exist:
- Late (silent) infection: this has few symptoms and can occur several years after implantation.
- A microabcess: more frequent than the above, they can form on stitches and are absorbed after their removal with local treatment.
- Toxic shock syndrome: rare cases of this have been reported.
• Skin necrosis: this occurs when tissue is starved of oxygen due to interruption of blood supply to the zone involved. This can be favored by high blood pressure, hematoma, an infection or heavy smoking by the patient. It is a rare complication but is formidable as, if serious; it can reveal the surface of the implant, notably by splitting the stitches. A second operation is often required, with possibly the need to remove the implant.
• Abnormal scar: formation the healing process is unpredictable, and scars can be less discreet than expected. They can be widened, retractile, hyper- or hypo-pigmented, hypertrophic, or rarely, keloid.
• Sensory changes: this is frequently found in the first few months but usually diminishes over time; rarely however, a certain degree of dysesthesia (heightening or diminution of sensitivity) can persist around the areola and the nipple.
• Galactorrhea/milk secretion: very rare cases of unexplained postoperative hormonal stimulation have been reported, giving rise to milk secretion which sometimes collects around the implant.
• Pheumothorax: very rare, has specific treatment.
2/ Specific implant-related risks
• Wrinkling or rippling: the implant is soft and natural, and for this reason the outer envelope of the implant can form creases, which can be palpable or visible in certain positions under the skin, giving a ‘ripple’, effect.
• Capsular contractures (Capsule): it is a normal physiological reaction that a fibrous shell should develop around an implant. A normal reaction to the presence of a foreign body in the organism is to isolate it from the foreign body with a hermetic membrane called a ‘periprosthetic capsule’. Normally this membrane is thin, supple and imperceptible but the reaction can increase and the capsule can thicken, become fibrous and contract exerting pressure on the implant, it is then known as a ‘capsule’. There are four stages of hardening that range from a normal undetectable aspect to severe forms giving hard, round, immobile breasts which can be painful.
Capsular contraction can follow infection or a hematoma, but often has no determined cause, resulting from unpredictable organic reaction.
Surgical techniques have made great progress in recent years, but especially the design and products used for the implants are much improved, this means a considerable reduction in the number of cases of capsular contraction and their seriousness.
If necessary, the capsule can be incised in a surgical procedure (capsulectomy).
• Rupture & leak: we have seen that implants have a limited life-span. An implant can become porous and the silicone rubber envelope of the implant can deteriorate. It can become porous, have tiny leakages or split. This can be rarely after an accident, a puncture with a needle or because of a manufacturing flaw. Much more often, however this is due to deterioration of the implant over time.
In all cases this will result in a leakage of the filling product, with different consequences according to the product concerned:
If the implant is filled with physiologic solution, the implant will deflate totally, either suddenly or slowly.
With silicone gel (non-resorbable) this will remain inside the membrane surrounding the implant. This can cause capsule formation or can remain un-noticed.
In some cases, much rarer now, (mainly because the modern gels are more cohesive), the gel can penetrate the surrounding tissue. Rupture of the implants usually requires an operation to change them. These are the facts that we wish to bring to your attention in all scientific fairness, concerning augmentation mammography.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unknown factors.
You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill requires to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation.
Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Breast Lift, Mastopexy of Reduction
The aim of this page is to give you all the essential information you need in order to make an informed decision, with full knowledge of the facts related to this procedure. Consequently, we strongly advise you to read it carefully.
Principles
Breast ptosis is the weighing of the breast gland causing a stretching of the surrounding skin and a global sagging of the breast. The breast lies in a too low position and is flattened in its upper part.
Breast ptosis can be present from the start, or appear after weight loss or pregnancy with breast feeding. It can be isolated (pure ptosis) or associated to mammary hypertrophy.
Conversely, there can be a ptosis with a small breast (hypoplasia or hypotrophic).
The aim of this operation is to elevate the nipple and areola to a more youthful position, tighten the gland and remove excess skin (and excess mammary gland) in order to obtain lifted and harmoniously shaped breast.
The operation shapes the breast by stretching the skin envelope and concentrating the glandular tissue. The gland is concentrated and put back in proper position, after removal of the skin excess, thus placing the nipple and areola back in a youthful position
The skin incisions are sutured and cause scars.
When the ptosis (or the hypertrophy) is very severe, the scars have an anchor shape, with a peri-areolar scar between the brown and white skin, a vertical scar from the areola down to the bottom fold of the breast (infra-mammary fold). The length of the horizontal scar is proportional to the severity of the sagging.

3 scars
When the ptosis is milder, an isolated vertical scar method can be used, thus avoiding the horizontal scar in the bottom fold and leaving only the peri-areolar and vertical scars.
2 scars
In some very mild breast ptosis, it is possible to use a concentric (or doughnut) mastopexy, which leaves only one scar around the areola.
Finally, in case of a too small breast volume (mammary hypoplasia), breast implants can be added, to restore a satisfying breast volume. In this case, it is usually possible to remove the excess skin around the areola and reduce the scar only to a peri-areolar scar.
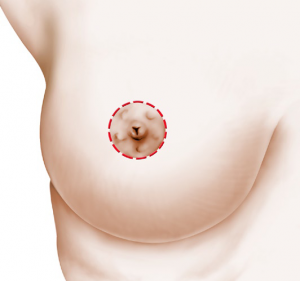
1 scar
Mammoplasty may be performed from the end of adolescence, when growth has ended, throughout life.
A further pregnancy or breast-feeding are possible, but we advise to wait for a minimum of 6 months after surgery.
Before The Operation
A preoperative check-up is made according to your surgeon’s recommendations.
You will meet the anaesthesiologist in consultation at latest, 48 hours prior to surgery.
Besides the usual preoperative examinations, your surgeon might ask you to have a mammogram (breast x-ray) or a breast ultra-sonography
No medication containing aspirin will be taken for 10 days before surgery & 3 days after surgery.
Stop smoking is recommended at least one month before and 6 weeks after the intervention (smoking can cause a delay or bad healing & others).
Type of Anesthesia
Breast reduction mammoplasty is usually performed under general anaesthesia. You will be asleep through the entire operation.
The Procedure
Every surgeon has his or her personal technical habits which he or she adapts to every new case, in order to obtain the best possible results. However, there are common principles:
All removed tissues are sent to a special laboratory for microscopic examination (histological exam).
Drains:
Two drains may be left in place for a few days after the procedure in order to evacuate any blood or liquid which may form.
After surgery, you will wear a special surgical “bra” day and night for 4 weeks; which size will have been determined in the consultation before the operation.
Depending on your surgeon and the severity of your ptosis, the operation can last two to three hours.
After The Operation
In most cases, postoperative pain is moderate and usually relieved by ordinary pain medication.
Swelling (edema), bruising and pain when lifting arms upwards are common symptoms.
You will leave the hospital 1 day after the operation and attend consultation few days later.
Your stitches, if not dissolvable, will be removed 8 to 21 days after surgery.
You should expect 7 to 15 days convalescence before returning to work.
You are advised to wait for one to two months before practicing any sports.
However, before this final outcome, one should be patient, wait for scars to slowly fade, and accept a regular follow-up every 3 months during one year.
The operated breast remains natural and sensitive and responds normally to hormonal shifts.
Disappointing Result
The main concern is scars, which will be closely looked after by your physician. They can often be red and swollen for 2-3 months. Then, they slowly fade away and with time, become moderately visible. However they can remain widened, clear or conversely, brown.
Regarding scars, it must stress that even though they usually fade away with time, they never completely disappear. If the surgeon controls sutures, scarring is a patient related process.
You may also notice a breast asymmetry, regarding volume, height, and size or nipple orientation. All these imperfections can be corrected secondarily, after one or two years.
Possible Complications
Mastopexy, even if performed for aesthetic reasons, is a genuine surgical procedure, with the consequent risks related to all medical acts, no matter how mild they might appear.
Post-operative care is usually simple after a Mastopexy. However, complications may occur: some are general, inherent to every surgical act, others are local and most commonly occur in very large breasts.
There are surgical and anaesthetic complications.
Concerning anaesthesia, the anaesthesiologist will inform you about all the anaesthetic risks. You must be aware that anaesthesia can sometimes cause unpredictable body reactions that can be difficult to control. The presence of an experienced anaesthesiologist, in a surgical environment, means that the risks are statistically practically negligible.
In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, offering optimal safety, especially when the operation is elective and the patient is in good general health.
Concerning surgery: By choosing a competent and qualified Plastic Surgeon, experienced in performing this procedure, you limit but do not entirely eliminate surgical risks.
Fortunately, genuine complications are rare after a properly performed mammoplasty. In fact, the vast majority of operations meet the patient’s satisfaction.
Among possible complications, you must be aware of the following:
• Infection can be treated with drainage and antibiotics.
• Blood clots (haematomas) are quiet rare but can occur. They can be evacuated.
• Localised skin or gland necrosis is rare with modern techniques. They can cause delayed healing.
• Numbness of the nipples may be observed. It is usually transient and most patients recover normal nipple feeling after 6 to 18 months.
. Delayed scar healing, hypertrophic scars , skin rejection or hypersensitivity to the dissolvable sutures after few days or weeks.
Most important to consider is the evolution of scars. These may sometimes become hypertrophic or bumpy (keloid), in a totally unpredictable manner, thus compromising the final aesthetic outcome. Such pathological scars may require long and specific local treatments.
In most cases however, this operation when correctly planned and executed, does offer very satisfying results in terms of comfort and well being, even if scars are inevitable and remain its major drawback.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors.
You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation.
Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia